
A new study funded by the National Institutes of Health (NIH) has established a significant link between exposure to particulate air pollution and increased mutation rates in lung cancers among individuals who have never smoked. This research, published [Insert Journal Name Here], provides compelling evidence that environmental factors play a crucial role in the development of lung cancer, even in the absence of traditional risk factors like smoking. This article will delve into the specifics of the NIH study, examining its methodology, key findings, and the implications for public health and future research into the mechanisms driving non-smoking lung cancer.
Table of Contents
- Particulate Matter Exposure Drives Distinct Mutation Patterns in Lung Adenocarcinoma
- Non Smokers Face Heightened Lung Cancer Risk From Airborne Pollutants
- Specific Air Pollutants Identified as Primary Mutagenic Agents
- Mitigation Strategies and Public Health Recommendations to Reduce Mutation Risk
- Q&A
- In Retrospect
Particulate Matter Exposure Drives Distinct Mutation Patterns in Lung Adenocarcinoma
Groundbreaking research funded by the National Institutes of Health (NIH) has identified a clear link between exposure to particulate matter (PM) air pollution and specific genetic mutations in lung adenocarcinomas, particularly among individuals who have never smoked. This study deepens our understanding of the mechanisms by which air pollution contributes to lung cancer development, highlighting the need for stricter air quality regulations and targeted prevention strategies. The findings suggest that these mutations are not random but rather a consequence of the inflammatory response triggered by prolonged exposure to fine particulate matter, which can subsequently damage DNA and disrupt normal cellular processes. As urban areas continue to grapple with rising air pollution levels, understanding these pathways becomes critical for early detection and intervention.
The research team meticulously analyzed tumor samples and environmental data, revealing recurring mutation patterns associated with different levels and compositions of PM exposure. These mutations were enriched in genes involved in critical cellular pathways, such as DNA repair and cell cycle regulation. This new information not only improves our understanding of how lung adenocarcinoma develops but also provides potential targets for personalized medicine and chemoprevention. Here’s a simplified breakdown of key findings:
- Specific PM types linked to distinct mutation profiles.
- Mutations found in genes regulating DNA repair mechanisms.
- Increased mutation burden correlated with higher PM exposure levels.
| PM Component | Associated Mutation |
|---|---|
| Black Carbon | KRAS |
| Sulfate | EGFR |
| Nitrates | TP53 |

Non Smokers Face Heightened Lung Cancer Risk From Airborne Pollutants
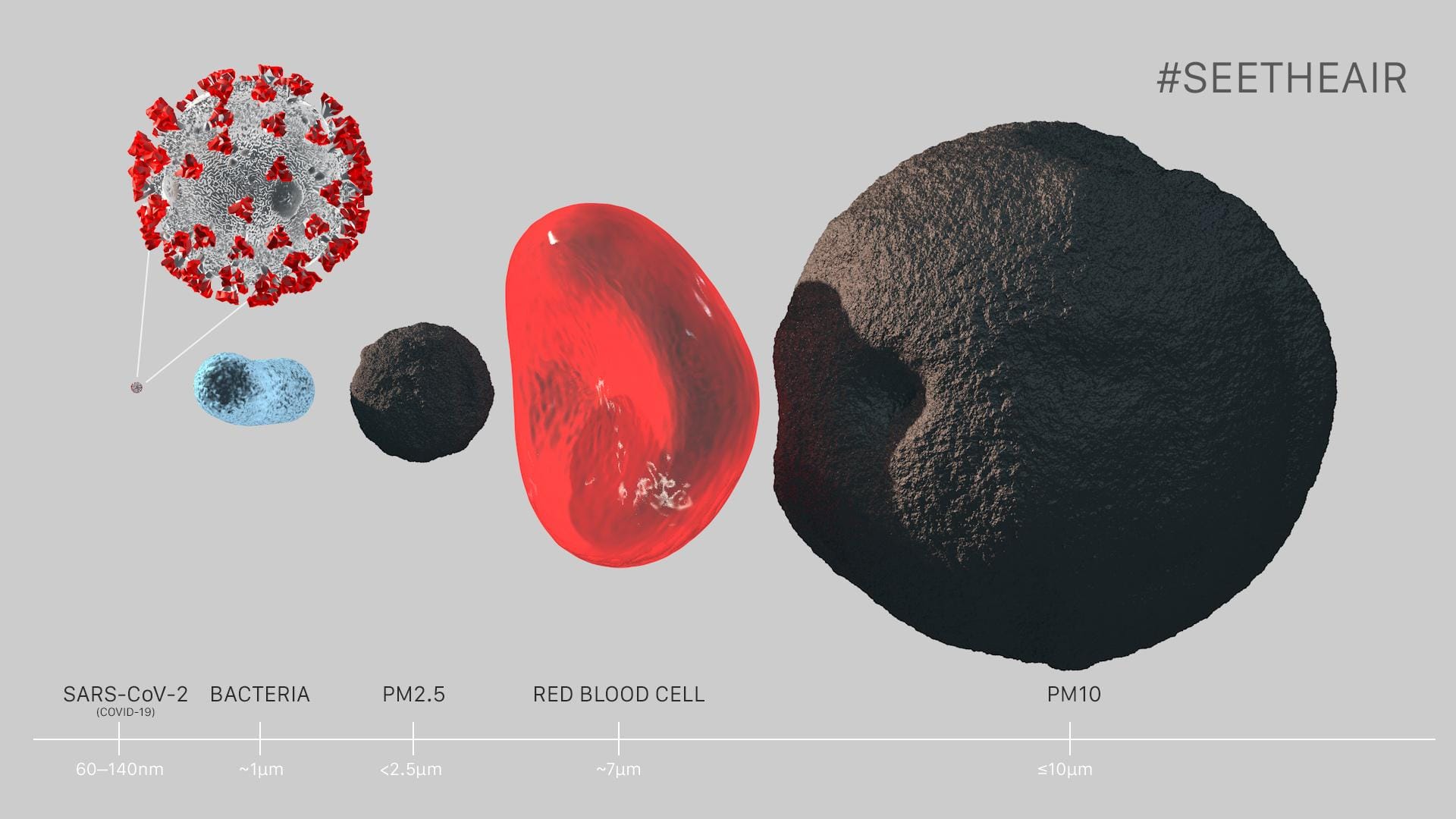
A groundbreaking new study funded by the National Institutes of Health (NIH) has revealed a concerning link between particulate air pollution and an increased risk of lung cancer, specifically in individuals who have never smoked. Researchers discovered that exposure to fine particulate matter (PM2.5), a common component of air pollution, can trigger genetic mutations that promote the development of lung tumors in nonsmokers. This finding challenges the long-held assumption that smoking is the primary driver of lung cancer and highlights the significant impact of environmental factors on public health. The study analyzed tumor samples, revealing a striking correlation between PM2.5 exposure and the prevalence of specific gene mutations commonly found in lung cancers.
The implications of this research are far-reaching, suggesting that even at levels currently considered “safe” by regulatory agencies, particulate air pollution poses a significant cancer risk. The study underscores the urgent need for stricter air quality regulations and mitigation strategies to protect vulnerable populations. Further research is crucial to fully understand the mechanisms by which PM2.5 causes these mutations and to develop targeted interventions. Here’s a breakdown:
- PM2.5: Fine particulate matter found in air pollution.
- Mutations: Changes in DNA linked to cancer development.
- Nonsmokers: Individuals who have never smoked.
| Pollutant | Health Risk |
|---|---|
| PM2.5 | Lung Cancer (Nonsmokers) |
| Ozone | Respiratory Issues |
| Nitrogen Dioxide | Asthma |
Specific Air Pollutants Identified as Primary Mutagenic Agents
The NIH study highlighted specific components within particulate matter as being particularly potent drivers of mutations observed in lung tumors of individuals who had never smoked. These culprits aren’t a single entity, but rather a complex mixture of compounds arising from various combustion processes. While the exact composition can vary geographically and seasonally, some key players consistently emerge as significant contributors.
Researchers pinpointed several groups of chemicals and specific elements commonly found in urban air that can potentially damage DNA. Key mutagenic agents include:
- Polycyclic Aromatic Hydrocarbons (PAHs): Byproducts of incomplete combustion, often associated with vehicle emissions and industrial processes.
- Black Carbon: A component of soot, arising primarily from diesel engines and biomass burning.
- Heavy Metals: Trace amounts of metals like nickel, chromium, and arsenic, often present in industrial emissions and coal combustion.
| Pollutant | Primary Source | Potential Effect |
|---|---|---|
| PAHs | Vehicle Exhaust | DNA Damage |
| Black Carbon | Diesel Engines | Cell Mutation |
| Heavy Metals | Industry | Increased Cancer Risk |

Mitigation Strategies and Public Health Recommendations to Reduce Mutation Risk
The troubling findings from the NIH study underscore the urgent need for proactive measures to combat particulate air pollution. Individuals can play a vital role in minimizing their exposure. Consider these steps:
- Monitor Air Quality: Regularly check local air quality indices and limit outdoor activities on high pollution days.
- Indoor Air Purification: Utilize high-efficiency particulate air (HEPA) filters in homes and offices to remove airborne particles.
- Protective Measures: Wear appropriate masks (N95 or equivalent) when exposure to polluted air is unavoidable.
- Advocate for Change: Support policies that promote cleaner air and stricter emissions standards.
On a larger scale, public health recommendations are crucial for mitigating the mutation risk associated with particulate air pollution. This is a multi-faceted problem that requires both short-term and long-term solutions, incorporating various sectors as follows:
| Sector | Recommendation |
|---|---|
| Transportation | Invest in electric vehicle infrastructure. |
| Industry | Implement stricter emission controls. |
| Energy | Transition to renewable energy sources. |
| Public Awareness | Educate on pollution health risks. |
Q&A
Q&A: New NIH Study Links Particulate Air Pollution to Lung Cancer Mutations in Non-Smokers
A groundbreaking NIH study has found a significant link between exposure to particulate matter (PM2.5) air pollution and specific gene mutations in lung cancers found in non-smokers. This research sheds new light on the complex factors contributing to lung cancer development beyond smoking. To help understand the implications of this study, we’ve compiled a Q&A with leading experts in the field.
Q: What is particulate matter (PM2.5) and why is it a concern?
A: PM2.5 refers to fine inhalable particles with a diameter of 2.5 micrometers or less. These particles are so small they can travel deep into the lungs and even enter the bloodstream. Common sources include combustion processes such as vehicle exhaust, industrial emissions, and burning wood. PM2.5 exposure is linked to a range of health problems, including respiratory illnesses, cardiovascular disease, and now, as shown in this study, an increased risk of specific lung cancer mutations.
Q: What specific gene mutations were found to be linked to PM2.5 exposure in the NIH study?
A: The study identified specific mutations in genes such as EGFR and KRAS, which are known to be frequently mutated in lung cancers found in non-smokers, particularly adenocarcinoma. The research indicated a strong correlation between higher levels of PM2.5 exposure and the prevalence of these specific mutations in the study participants diagnosed with lung cancer.
Q: How did the researchers determine that PM2.5 was a significant factor, especially considering other potential environmental influences?
A: The researchers used sophisticated statistical modeling and data analysis techniques to account for other known risk factors for lung cancer, such as genetic predisposition, occupational exposures, and second-hand smoke. By controlling for these variables, they were able to isolate the association between PM2.5 exposure and the observed prevalence of EGFR and KRAS mutations. They also analyzed data from multiple large prospective studies involving diverse populations, further strengthening the evidence.
Q: Does this study mean that everyone exposed to PM2.5 will develop lung cancer?
A: No. It’s crucial to understand that this study identifies an increased risk of specific lung cancer mutations among those exposed to PM2.5. It does not mean that exposure guarantees lung cancer development. Lung cancer is a complex disease, and multiple factors contribute to its development. This study highlights PM2.5 as a previously underappreciated contributor, particularly in non-smokers.
Q: What are the key implications of this research for public health?
A: This study underscores the significant impact of air pollution on public health, extending beyond respiratory and cardiovascular concerns to include cancer risk. It provides further justification for strengthening air quality regulations and promoting measures to reduce PM2.5 emissions from various sources. It also highlights the importance of continued research into the mechanisms by which PM2.5 contributes to lung cancer development, which could lead to new prevention and treatment strategies.
Q: What steps can individuals take to minimize their exposure to PM2.5?
A: While large-scale solutions require policy changes and industrial regulation, individuals can take steps to reduce their exposure. These include:
Monitoring air quality reports: Pay attention to air quality indices and avoid outdoor activities on days with high PM2.5 levels.
Using air purifiers: Employing air purifiers with HEPA filters in homes and workplaces can help remove PM2.5 from indoor air.
Minimizing exposure to traffic: Avoiding heavily trafficked areas during peak hours can reduce exposure to vehicular emissions.
Supporting policies that promote cleaner air: Advocate for and support policies that aim to reduce air pollution from industrial and transportation sources.
Q: What are the next steps researchers should take based on these findings?
A: Further research should focus on:
Elucidating the precise mechanisms: Investigating how PM2.5 exposure specifically triggers these genetic mutations in lung cells.
Identifying susceptible populations: Determining which individuals are most vulnerable to the carcinogenic effects of PM2.5.
Developing biomarkers: Creating biomarkers that can identify individuals at higher risk of developing lung cancer due to PM2.5 exposure.
Testing interventions: Evaluating the effectiveness of interventions, such as air pollution control measures, in reducing the incidence of these PM2.5-related lung cancers.
This study provides compelling evidence for the impact of air pollution on lung cancer risk in non-smokers. It emphasizes the need for continued efforts to improve air quality and further investigate the underlying mechanisms linking PM2.5 exposure to lung cancer development.
In Retrospect
In conclusion, this NIH study provides compelling evidence linking particulate air pollution, specifically PM2.5, to a distinct mutational signature in lung cancers diagnosed in individuals who have never smoked. These findings underscore the significant public health implications of air pollution exposure, even at levels previously considered relatively safe. Further research is needed to fully elucidate the mechanisms by which PM2.5 induces these mutations and to assess the long-term impact on cancer development and progression. Ultimately, these findings support the continued need for stringent air quality regulations and mitigation strategies to protect vulnerable populations and reduce the overall burden of lung cancer globally.




